CATARACT AND
ITS TREATMENT
|
| |
Sight
is our most precious sense enabling us to enjoy the beauty
of the world in which we live. For centuries, developing
cataract doomed a person to blindness.
|
| |
Today
modern microsurgical techniques allow people to enjoy good
clear vision after their cataracts have been removed. Giving
up favourite activities and suffering through years of
poor vision due to cataract is no longer an inevitable
part of the ageing process.
|
How
the Eye Works:
|
| |
Before
understanding cataract, it is important to know how a normal
eye works. The eye is like a camera. The lens in a camera
allows light to pass through and focuses that light on
the film at the back of the camera for a clear picture.
|
| |
The
eye works in a similar way. The lens of the eye is normally
clear and allows light to pass through. The light is focused
on a thin film-like retina, which is situated at the back
part of the eye. The image is transmitted to the brain
via the optic nerve. This is how we see.
|
| |
|
What
is a cataract?
|
| |
It
is a cloudiness of the normally clear lens in the eye.
It prevents the lens from focusing light onto the retina
and hence causes unclear vision. As the cataract advances,
this cloudiness of vision increases over a period of time
until the vision is completely impaired.
|
Why
does a cataract develop?
|
| |
Cataract
development is part of the normal ageing process. Almost
all people above the age of 60 years have cataract of a
variable degree, although it can occur at any age. In some
people cataract development is aggravated by an eye injury,
presence of diabetes, use of medications or other eye diseases.
|
| |
Rarely
cataract may be present in the newborn as a development
defect.
|
Symptoms
|
| |
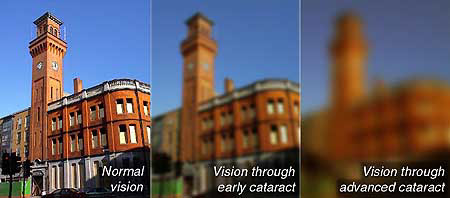 Because
cataracts form in different ways, the symptoms of cataracts
are variable. Most people notice that their vision gradually
deteriorates - objects may begin to look yellow, hazy
or blurred. Many people also find that they need more
light to see clearly, or that they experience glare or
haloes from lights at night. Other
common problems include increasing nearsightedness, double
vision or the appearance of dark spots or shadows in
the vision. In advanced cases, the cataract may be visible
as a white or yellowish-looking pupil (as seen below). Because
cataracts form in different ways, the symptoms of cataracts
are variable. Most people notice that their vision gradually
deteriorates - objects may begin to look yellow, hazy
or blurred. Many people also find that they need more
light to see clearly, or that they experience glare or
haloes from lights at night. Other
common problems include increasing nearsightedness, double
vision or the appearance of dark spots or shadows in
the vision. In advanced cases, the cataract may be visible
as a white or yellowish-looking pupil (as seen below).

|
Can
cataract be prevented or treated with medication?
|
| |
Cataracts
that occur due to the ageing process cannot be prevented
as the ageing process itself cannot be prevented. Using
the eyes for reading and similar activities have nothing
to do with cataract formation. Avoiding the use of eyes
will not prevent cataract.
|
| |
Till
date as per all authentic medical research no medication
exists to prevent or cure a cataract. The only known treatment
for cataract is surgery.
|
What
is Micro Surgery?
|
| |
An
eye operation performed with the help of a microscope is
called microsurgery. Intraocular Lens Implantation and
Phacoemulsification cannot be performed with precision
unless done with a sophisticated operating microscope.
|
When
can you have Cataract Surgery?
|
| |
Cataract
surgery can be performed as soon as the patient feels handicapped
in performing routine activities at work and leisure. In
modern times it is neither advisable to wait for the cataract
to mature (as it can lead to complications like glaucoma),
nor necessary, as we have access to "state-of-the-art" surgery.
For performing phacoemulsification it is desirable to get
surgery done before the cataract fully matures.
|
What
does cataract surgery entail?
|
| |
 It
is one of the oldest, safest and most successful forms
of surgery. It requires a very short hospital stay and
is generally performed under local anaesthesia. The patient
is awake during surgery but does not feel any discomfort
or pain. Patients are ambulatory and discharged immediately
after surgery. It
is one of the oldest, safest and most successful forms
of surgery. It requires a very short hospital stay and
is generally performed under local anaesthesia. The patient
is awake during surgery but does not feel any discomfort
or pain. Patients are ambulatory and discharged immediately
after surgery.
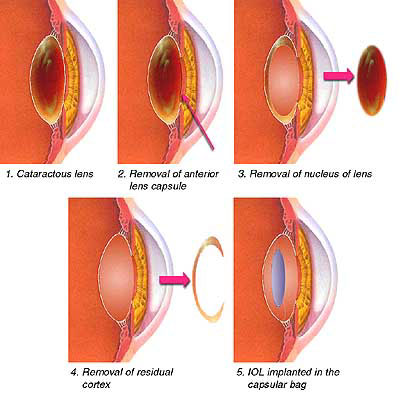
For
the surgery a small opening is made in the eyeball. The front
part of the lens capsule which is a thin membrane enclosing
the entire lens is cut, making a smooth round opening in
the front part of the capsule. All cloudy lens material is
removed by a routine cataract procedure or by phacoemulsification.
The
back of the lens capsule is left in place so that the artificial
lens implant will be able to rest securely within it. If
the lens capsule is not able to hold the implant it can be
placed in front of the iris i.e. the coloured part of the
eye. |
Are
there any problems with an I.O.L.?
|
| |
Fortunately
the technological advances in I.O.L. manufacture and surgery
have made it quite safe. Complications are rare and similar
ones can occur with conventional surgery without an I.O.L.
implantation. All patients irrespective of other general
illnesses like diabetes, hypertension etc. can have I.O.L.
surgery. If there is any reason why you should not have
an I.O.L. your ophthalmologist will explain.
|
Will
you need glasses after I.O.L. surgery?
|
| |
The
natural lens in the eye can change its shape to focus for
various distances. The I.O.L., since it is made of plastic,
cannot do so. Hence, glasses either of small plus or minus
power are usually needed to obtain best possible vision
following surgery. Since the I.O.L. calculations, by a
computerized ultrasound biometer, are based on certain
theoretical/regression formulae, it will vary on a person-to-person
basis. Although we expect very minimal post-operative power
in the glasses, some people may have a slightly larger
postoperative refraction than others. In some patients,
power of glasses in the operated eye is necessary for coordination
with the other eye.
|
What
is this new method of Cataract with I.O.L. surgery called
PHACOEMULSIFICATION? How is it different from Non-Phaco
Cataract with I.O.L. surgery?
|
| |
 Routine
cataract surgery requires an incision 11-12 mm in size.
Phacoemulsification is performed through a 1.4-2.75 mm
incision using a thin titanium probe, which emits high-speed
ultrasound waves, vibrating at 40,000 times per second.
This breaks the cataract into tiny pieces, which are then
aspirated or sucked out of the eye through the same probe. Routine
cataract surgery requires an incision 11-12 mm in size.
Phacoemulsification is performed through a 1.4-2.75 mm
incision using a thin titanium probe, which emits high-speed
ultrasound waves, vibrating at 40,000 times per second.
This breaks the cataract into tiny pieces, which are then
aspirated or sucked out of the eye through the same probe.
Small
and micro incisions such as those used in phacoemulsification
are preferable because they seal themselves immediately after
surgery and heal very quickly. It is only a reflection of
our unshakable commitment to quality that we are perhaps
the first institution in Delhi to acquire the Millennium
Phacoemulsification System, the latest top-of-the-line phacoemulsification
machine available in the world. We also now have the Alcon
Legacy Series 20000 Phacoemulsification System, as well as
the Sovereign Phacoemulsification System with WhiteStar technology
for delivering "Cold Phaco" which has the advantage of significantly
reducing the ultrasonic energy to break up the cataract.
A small incision causes less tissue damage and increases
surgical safety. No-stitch or one-stitch may be used in phacoemulsification
surgery whereas in Non-Phaco I.O.L. surgery, 6-8 crossed
stitches are used. These cause changing curvature of the
eyeball and hence a delay in the final spectacle prescription.
Another advantage of small incisions is that they are less
likely than other incisions to cause a focusing problem known
as astigmatism. The postoperative rehabilitation is faster
and you can return to your normal work and activities very
soon. This is currently the most effective method for removing
cataracts. |
| |
Keeping
pace with the advanced technology we are now coupling Phacoemulsification
with implantation of the best quality Foldable lntraocular
Lenses that can be inserted through even smaller incisions,
further increasing the benefits of phacoemulsification.
|
What
are Foldable Lenses?
|
| |
Following
phacoemulsification, the incision has to be slightly enlarged
to 5 mm or more to allow the non-foldable intraocular lens
to be inserted. However the latest concept of Foldable
Intraocular Lenses allows these lenses to be inserted through
as small an incision as 1.5-3.5 mm. Once inside the eye
the IOL unfolds and stays in place securely. However your
surgeon will decide which lens is most suited to your eye.
|
Phacoemulsification
with Non-Foldable Intraocular Lenses
|
| |
This
procedure is also available. It requires an incision that
is only slightly larger than that for a foldable intraocular
lens. The benefits are that it retains the advantages of
phacoemulsification while cutting down the cost of the
intraocular lens.
|
| |
|
Can
all patients having a cataract undergo Phaco surgery?
|
| |
Your
eye surgeon will be the best judge to decide whether you
can undergo
phaco-surgery.
 Each patient undergoing cataract surgery at our centre is examined
in detail to assess the endothelial count of the cornea
using the automated specular microscope. The endothelium
is the inner most layer of the cornea which is responsible
for its transparency. Preoperative assessment of the
endothelial count enables us to identify patients in
whom this layer is weaker (low cell counts), therefore
are not suitable for the phacoemulsification procedure,
and in whom surgery by the conventional technique would
be safer. Again based on findings of the endothelial
count by specular microscopy it may be necessary to alter
certain medication used at the time of surgery. If necessary
we are using BSS/BSS Plus and Healon/ Healon GV, which
are imported medicines, to minimize loss of the already
depleted endothelial cell counts during surgery. Each patient undergoing cataract surgery at our centre is examined
in detail to assess the endothelial count of the cornea
using the automated specular microscope. The endothelium
is the inner most layer of the cornea which is responsible
for its transparency. Preoperative assessment of the
endothelial count enables us to identify patients in
whom this layer is weaker (low cell counts), therefore
are not suitable for the phacoemulsification procedure,
and in whom surgery by the conventional technique would
be safer. Again based on findings of the endothelial
count by specular microscopy it may be necessary to alter
certain medication used at the time of surgery. If necessary
we are using BSS/BSS Plus and Healon/ Healon GV, which
are imported medicines, to minimize loss of the already
depleted endothelial cell counts during surgery.
Other
relative contraindications to having phacoemulsification
surgery would be very poorly dilating pupils, certain
corneal diseases and very hard cataracts as the amount
of energy required to break up the cataract would probably
damage the eye.
In
the above eyes, conventional cataract extraction with
intraocular lens implantation still remains a safe,
economical and effective method of treatment of cataract,
since the ultimate visual outcome in both the conventional
procedure and phacoemulsification are comparable. The
difference lies only in the rate of healing.
No
surgeon in the world can perform a surgery with guaranteed
results. However, almost all patients regain good vision
following cataract surgery. The calibre of vision obtained
after a successful cataract surgery with I.O.L. also depends
upon the health of other structures of the eye.
Eye
disease or problems in the cornea, retina or optic nerve
may limit the potential for clear vision even when the cataract
surgery itself has been successful. However, it might not
always be possible to evaluate the condition of the retina,
optic nerve, in advanced cataracts pre-operatively.
Phaco
or Non-Phaco Cataract with I.O.L. surgery is not a magica1
procedure and need not necessarily restore normal vision
immediately. Blurred vision is common immediately after surgery.
As the eye heals over a period of time, vision improves gradually. |
Can
Cataract be treated with Lasers?
|
| |
Contrary
to a popular myth cataract cannot be removed with lasers.
Surgery done by phacoemulsification is commonly termed "Laser
Surgery" by many people.
However,
in a large number of patients undergoing cataract surgery
by the modern technique, the back part of the lens capsule
thickens over a period of time and causes blurred vision.
This is known as a secondary cataract. This is not a complication.
The condition is treated with a "YAG Laser" with full restoration
of vision. |
Benefits
of cataract surgery:
|
|
|
There
are numerous benefits of cataract surgery, many of which
cannot be measured statistically. These include:
|
Improved
colour vision |
|
colours
are brighter and more vivid after cataract surgery. |
|
Greater
clarity of vision - vision is crisper and sharper after
cataract surgery. |
|
Improved
quality of life - studies have repeatedly shown that
people enjoy an improved quality of life after successful
cataract surgery. Many people can resume driving, reading,
writing, watching television, sewing, household work
and using a computer immediately after. Even when retinal
diseases or other problems prevent a total restoration
of vision, the remaining vision is usually improved
by cataract surgery. |
|